Transforming Denial Management with Data Analytics
How Aireimbursements Uses Power BI to Drive Revenue Cycle Efficiency
11/6/20252 min read
In today’s healthcare environment, financial performance is increasingly tied to how effectively organizations manage denials. Despite advancements in electronic billing and EHR integration, many providers continue to struggle with identifying the root causes of claim denials and preventing revenue leakage.
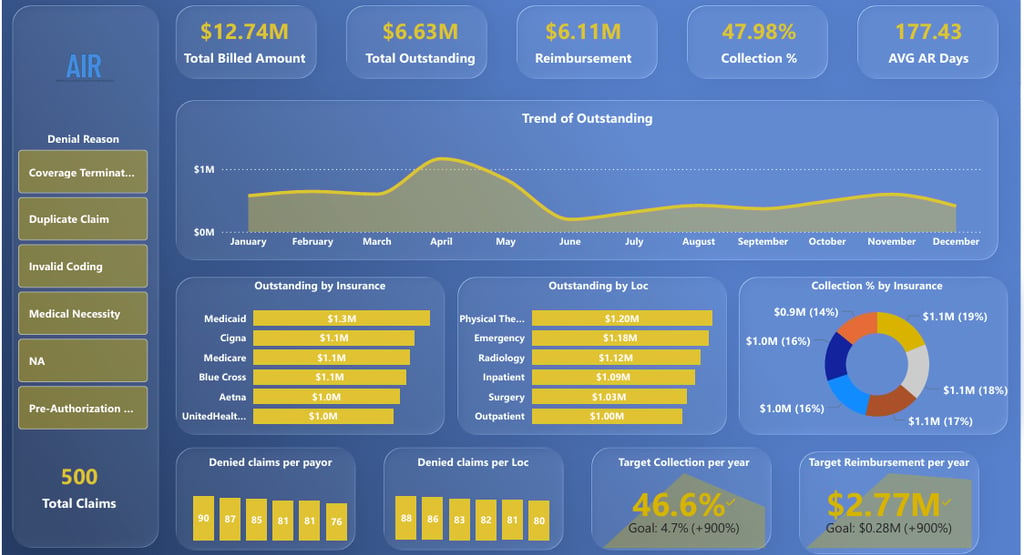
At Aireimbursements, we specialize in RCM data analytics that turn denial data into clear, actionable intelligence. Our recent AIR Report Dashboard, developed using Power BI, demonstrates how analytics can transform the way denial management teams track, analyze, and resolve outstanding claims.
The Denial Management Challenge
Every healthcare organization faces multiple categories of denials—each requiring a different strategy for resolution. Traditional reporting often lists denial volumes and balances, but it fails to provide meaningful insights into patterns or preventable causes. This results in repeated denials, lost revenue, and inefficiencies in the AR process.
Our team designed the AIR Report Dashboard to break through that limitation. By categorizing denials based on their root causes and linking them with specific actions, teams can move from reactive follow-up to proactive resolution.
Insights from the AIR Report
The dashboard provides a consolidated view of denial categories, outstanding balances, and actionable next steps. Below are some of the key findings from our sample dataset:
Policy Inactive
96 claims totaling $1.2 million in outstanding balance
Requires verification of policy effective and termination dates
Collaboration between AR teams to confirm patient coverage before resubmission
Duplicate Claims
83 claims totaling $1.1 million in outstanding balance
Analysis focuses on identifying corrected claims and ensuring proper TOB/IP billing within the 72-hour rule
Invalid Coding
73 claims with $900,000 in outstanding balance
Coding errors found primarily in emergency and radiology services
Insights used to coordinate with coding teams for corrections and resubmissions
Authorization Denials
83 claims with $1.1 million in outstanding balance
Significant portion linked to emergency claims not requiring prior authorization
Workflow includes reprocessing and verification for retro authorizations
Medical Necessity
90 claims totaling $1.2 million denied for medical necessity reasons
IP claims represent the majority, requiring appeals with supporting clinical documentation
NA (No Reason Found)
75 claims totaling $1 million
Requires manual review by AR analysts to classify and resolve denial causes
Turning Data into Action
The true strength of the AIR Report lies not only in displaying data but in driving action. Each denial category is mapped to a specific resolution workflow—ensuring accountability, measurable follow-up, and faster turnaround times.
By integrating automation and visualization, Aireimbursements enables AR teams to:
Prioritize high-impact denial categories
Assign claims to the appropriate departments
Track resolution progress in real-time
Identify recurring patterns for process improvement
This structured approach helps organizations reduce rework, accelerate collections, and improve their overall clean claim rate.
Impact on Revenue Cycle Performance
Implementing data-driven denial management has shown measurable benefits:
Reduction in denial resolution time by identifying patterns early
Improved collaboration between billing, coding, and AR departments
Better forecasting of potential revenue risk
Enhanced visibility for leadership through performance dashboards
Healthcare organizations that leverage analytics in denial management gain a significant competitive advantage. They are better equipped to control AR aging, improve compliance, and ultimately, strengthen their financial sustainability.
The Aireimbursements Advantage
At Aireimbursements, we combine deep RCM expertise with data analytics capabilities to help healthcare providers turn complex financial data into operational excellence. Our Power BI-based solutions are fully customizable to each client’s workflows, EHR systems, and reporting needs.
We don’t just present data — we deliver actionable insights that drive measurable results.
To learn more about how Aireimbursements can help your organization optimize denial management through data analytics, contact us at Ai.Reimbursments@outlook.com.
Aireimbursements – Empowering Healthcare Revenue with Data.
Help
Questions? Reach out anytime.
Contact
Connect
+91-7418551160
© 2025. All rights reserved.
Ai.Reimbursements@outlook.com